Patellar Instability
Description:
The knee joint is composed of three bones: the kneecap (patella), thigh bone (femur), and shin bone (tibia).
The back of the kneecap has a ridge on it called the patellar ridge; the front of the thigh bone has a groove in it, called the trochlea. The ridge of the patella slides up and down in the trochlea as the knee flexes and extends. The shape of 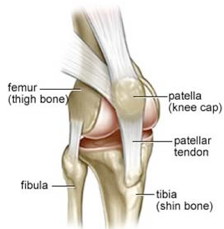 the ridge and groove helps to stabilize the kneecap during knee range of motion.
the ridge and groove helps to stabilize the kneecap during knee range of motion.
Here is an x-ray depicting the kneecap (patella) resting in the trochlear groove of the thigh bone (femur).
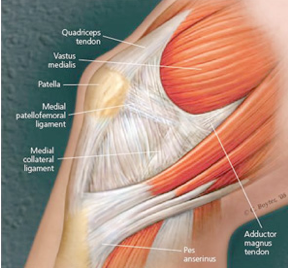
In addition to the bony anatomy of the kneecap and the thigh bone, the kneecap is also stabilized in the center of the groove by soft tissues, including ligaments and muscles. The main ligamentous soft tissue stabilizer of the knee is called the medial patellofemoral ligament (MPFL).
The kneecap is also stabilized by the dynamic actions of the quadriceps muscle and tendon; the quadriceps is a group of four muscles including the vastus medialis, vastus intermedius, vastus lateralis, and rectus femoris.
Patellar instability is a condition that occurs when the kneecap comes out of the groove. When the kneecap comes completely out of the groove this is called a dislocation; when the kneecap comes partially out of the groove this is called a subluxation.
Here is a clinical photograph showing a patient with a patellar dislocation.
 Patellar instability can occur following an acute traumatic episode, such as a sudden twisting injury to the knee.
Patellar instability can occur following an acute traumatic episode, such as a sudden twisting injury to the knee.
Patellar instability can also occur in the absence of an injury in a patient who has an anatomic predisposition to patellar instability. Factors which predispose to patellar instability include weakness or atrophy of the vastus medialis muscle, a shallow trochlear groove, an abnormally shaped patella with no patellar ridge, ligamentous laxity or soft-tissue hypermobility disorders, such as Ehlers-Danlos syndrome, or other abnormal anatomic configurations involving the interaction between the femur (thigh bone) and tibia (shin bone).
Signs & Symptoms:
Patients with a patellar dislocation report obvious deformity and displacement of the kneecap relative to its normal position. Typically, however, patients do not complain of pain between instability episodes.
Diagnosis:
The diagnosis of patellar instability is typically made by a combination of the patient’s history, the findings on physical examination, and imaging studies, which may include x-rays, a CT scan, and possibly an MRI.
Treatment:
Treatment for patellar instability depends upon the nature of the instability (dislocation versus subluxation), the number of instability episodes sustained by the patient, the presence of anatomic predisposing factors to patellar instability, the existence of associated injuries in the knee, and the response to previous treatments.
For patients with first time dislocation events, typically conservative treatment including short-term immobilization, bracing, and physical therapy are recommended.
Despite these treatment modalities, the rate of recurrent instability episodes ranges from 15-44%. For patients who suffer from debilitating recurrent instability episodes that have failed to respond to non-operative treatment measures, surgical treatment may be considered.
The nature of the surgery depends upon the quality of the soft tissue stabilizers (including the MPFL and vastus medialis) as well as the patient’s bony anatomy. The surgery may either be a soft tissue procedure, a bony procedure, or a combination of both.
