Approximately 50 percent of all knee injuries involve either a partial or complete tear of the anterior cruciate ligament (ACL). Surgical reconstruction is done to repair this ligament when this occurs. One technique that is popular is the allograft bone-patellar tendon-bone procedure. This is the alternative to the autograft procedure, which can lead to in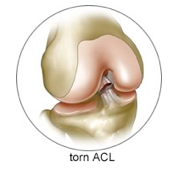 creased morbidity.
creased morbidity.
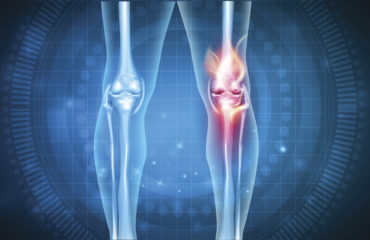
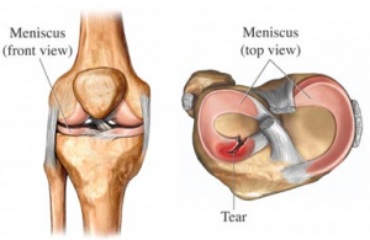
The ACL is the main stabilizer of the knee joint, but it is one of the most frequently injured ligaments, particularly for athletes. The ACL is also injured in motor vehicle accidents and injuries in the home and/or workplace. When this type of injury occurs, surgical reconstruction is done to restore normal knee function and to protect other structures of the knee.
During the last 30 years, surgery for a torn ACL has advanced tremendously with a success rate of around 90 percent. Because the ACL cannot be repaired following a rupture, it must be replaced with another structure. This means that tunnels should be made in the bone at the attachment sites so the replacement tissue can be fixed to the bone. It is fixed to the bone with various devices, such as pins, staples, or screws.
The Procedure
The common tissues used as ACL grafts are the middle third of the patellar tendon, which has a small piece of bone from the patella on one end and a tibia attachment on the other end. Also, the hamstring tendons, quadriceps tendon, or iliotibial band is 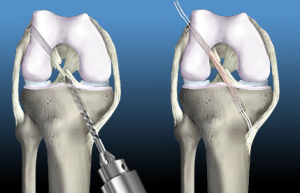 also used. The allograft tissue comes from the patellar tendon (knee), tibialis tendon (ankle), or achilles tendon (heel). During the ACL bone-patellar bone-tendon reconstruction, a small piece of bone from the patella on one end of the tibia attaches to the other end. The repair is held together by metal or screws as the bone segments heal with the tissue.
also used. The allograft tissue comes from the patellar tendon (knee), tibialis tendon (ankle), or achilles tendon (heel). During the ACL bone-patellar bone-tendon reconstruction, a small piece of bone from the patella on one end of the tibia attaches to the other end. The repair is held together by metal or screws as the bone segments heal with the tissue.
During the healing time, protective exercise is performed so there is no damage to the reconstruction. The first week of post-operatively requires rest, and patients are advised to apply ice to the affected area. Once in a rehabilitation program, a continuous passive motion (CPM) machine is used to help with knee strengthening.
Extension and full knee straightening is the main goal following the procedure. To achieve this, pillows are used underneath the heel at rest, and patients should not put a pillow underneath the knee. During the first month, a knee immobilizer is used to protect the knee. Patients can return to full sports and activities within six months of the operation.
Pros and Cons of the Bone-Patellar Tendon-Bone Graft
The pros of the bone-patellar tendon-bone graft include well-proven, long-term clinical success, easy and comfortable rehabilitation, Scottsdale orthopedic surgeons are familiar with this technique, and it provides strong early fixation with bone against bone.
However, the cons are that this procedure requires a larger incision, there may be residual weakness of the quadriceps muscles, there is a risk of patella fracture following surgery, and there is a higher incidence of long-term knee pain and trouble with kneeling.