Knee tendon bursitis results from trauma, degenerative joint disease, and overuse. This condition affects the inner knee (medial aspect). This painful condition affects obese women, athletes, and older adults with arthritis.
What structures are affected with knee tendon bursitis?
Pes anserinus means “goosefoot,” which is used to describe the appearance of conjoined tendons that attach to the inner aspect of the tibia (shin bone). Below the pes anserinus tendons is the bursa, which is called the pes anserine. This bursa functions as a cushion-like sac holding fluid to allow the tendons to smoothly glide over the bone.
What causes pes anserinus bursitis?
Knee tendon bursitis is caused by inflammation of the bursa. This occurs due to trauma, arthritis, degenerative joint disease, trauma, and obesity. Several factors contribute to development of knee tendon bursitis, including:
- Obesity
- Arthritis of the knee
- Tight hamstring muscles
- An out-turning knee and leg
- Incorrect training techniques (neglecting to stretch, sudden increase in mileage)
- Medial meniscus tear
Is knee tendon bursitis common?
In a large review of studies involving over 500 patients who had MRI studies of the knee, the researchers found that knee tendon bursitis was detected in 2.5% of patients. The most common clinical presentation was pain along the inner joint line. The incidence of pes anserinus bursitis is highest among:
- Middle-aged women who are overweight or obese.
- Young athletes who participate in activities that require abrupt side-to-side cutting or motions, such as tennis, soccer, and basketball.
- Older adults with arthritis.
- People with flat feet
- People who have a bow-leg knee deformity.
What are the symptoms of knee tendon bursitis?
Knee tendon bursitis causes pain with certain movements, tenderness, and swelling. Activities that lead to pain include climbing stairs and rising from a sitting position.
How is knee tendon bursitis diagnosed?
The doctor diagnoses knee tendon bursitis by reviewing the medical history and examining the knee. The doctor may use x-rays, ultrasounds, and MRI scans to confirm the diagnosis and rule out serious knee injuries.
How is knee tendon bursitis treated?
Treatment options include:
- RICE protocol – This involves rest, use of ice packs, wearing a compression bandage, and elevating the affected leg.
- Physical therapy – This involves use of exercise, icing, and therapeutic ultrasound to restore function and relieve pain. In addition, therapy is used to strengthen muscles, which can occur from disuse of the knee.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) – These are used to decrease pain and alleviate swelling related to inflammation.
- Injection – The doctor may inject a solution of corticosteroid and anesthetic into the bursa, which usually provides prompt relief.
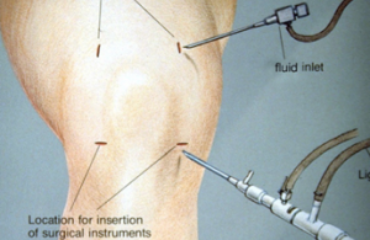
- Surgery – This involves removal of the bursa and any bony growths on the joint area. Following surgery, you must use crutches and cannot return to activities for around 6 weeks.
When can the athlete return to activities?
Returning to rigorous activities and running is not recommended until the bursa and tendon are free of pain. A graded return to activities should begin with short duration jogging for around 10 minutes initially. This can be increased, with a minimum of 2 days rest between runs.
For the top sports medicine treatment in Phoenix, Dr. Adam Farber provides both nonoperative and operative options for patients. This includes medications, physical therapy, bracing, and minimally invasive surgery with arthroscopic techniques. Call today!
Resources
Alvarez-Nemegyei J, Canoso JJ. Evidence-Based Soft Tissue Rheumatology IV: Anserine Bursitis. J Clin Rheumatol. 2004 Aug. 10(4):205-6.
Helfenstein M Jr, Kuromoto J. Anserine syndrome. Rev Bras Reumatol. 2010 May-Jun. 50(3):313-27.
Rennie WJ, Saifuddin A. Pes anserine bursitis: incidence in symptomatic knees and clinical presentation. Skeletal Radiol. 2005 Jul. 34(7):395-8. [Medline].