The shoulder is a ball-and-socket joint that is shallow. Because this joint is shallow, it is more mobile than other joints. However, this great range of motion can also cause joint problems. Shoulder instability occurs when the ball moves around too freely in the socket.
What are the main shoulder components?
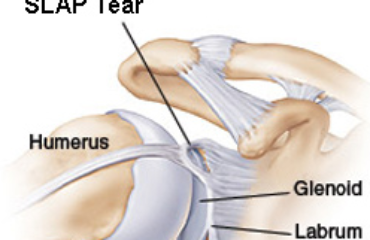
The socket of the shoulder is called the glenoid cavity. This cavity is circled by a ring of tissue called the labrum. The  humerus (upper arm bone) has a head (the ball) that fits neatly into the socket. This joint is stabilized by a group of ligaments that stretch to allow shoulder movement, as well as tighten to prevent too much motion. Tendons and muscles also surround the shoulder to provide support and stability.
humerus (upper arm bone) has a head (the ball) that fits neatly into the socket. This joint is stabilized by a group of ligaments that stretch to allow shoulder movement, as well as tighten to prevent too much motion. Tendons and muscles also surround the shoulder to provide support and stability.
What causes shoulder instability?
The joint capsule is slightly loose, but for a flexible person, it tends to be looser. Overuse in certain sports (baseball, volleyball and swimming) causes the capsule to stretch and become too lax. When this occurs, the shoulder muscles weaken, and the ball of the humerus starts to slip around in the socket.
An extreme case of shoulder instability is dislocation, which occurs usually due to a traumatic event. When a shoulder dislocates, the head of the humerus comes out of the socket, and tears away from the labrum (Bankart tear). A Bankart tear makes the shoulder easier to dislocate, as the labrum acts as a bumper to keep the humeral head in position.
Who has chronic shoulder instability?
People between the ages of 19 and 29 years are more likely to experience recurrent and chronic shoulder instability. The recurrence rate for these patients is around 60%, according to studies. The recurrence rate for persons in their 30s and 40s is only around 20%.
What are the symptoms of shoulder instability?
Symptoms of shoulder instability include:
- A sensation of looseness of the shoulder joint
- Shoulder feels like it is coming out of place
- Shoulder pain with activity
- Development of secondary conditions, such as bursitis, tendinitis, and inflammation (occurs due to excessive motion and irritation to shoulder structures)
How is shoulder instability diagnosed?
The doctor can usually diagnose shoulder instability with a medical history and physical examination. The doctor will as you questions about your symptoms, inquire of your activities, and make you move your shoulder through range of motion. X-rays are used to detect deformities of the bones and shoulder dislocation. IF the doctor is concerned about a Bankart tear, or a stretched joint capsule, he may order a magnetic resonance imaging (MRI) scan.
How is shoulder instability treated?
Shoulder instability with no history of dislocation usually responds to non-surgical measures, but surgery may be required. Treatment options are:
- Physical therapy – Used to strengthen the shoulder girdle muscles, which are part of the shoulder’s stabilizing forces. Improving strength will create a more efficient joint and reduce joint capsule stretching, which occurs with activity. The therapist will also use various pain relief measures, such as electrical stimulation, ultrasound, and massage.
- Rest and ice – The doctor may recommend that you rest your shoulder joint for a few days or weeks. Ice is used to relieve pain and decrease inflammation. You can apply an ice pack for 20-minute intervals several times each day.
- Corticosteroid injection – The doctor can inject the shoulder with a corticosteroid agent, which reduces inflammation.
- Arthroscopy – If the shoulder remains unstable after conservative measures, or if pain continues, the Scottsdale orthopedic doctor can perform an arthroscopic procedure. This involves insertion of a thin, optic camera into the shoulder joint to diagnose and treat the instability. During the procedure, the torn labrum is reattached to the glenoid using anchors, sutures, and wires, which recreates the bumper effect and prevents the ball from slipping around. If the capsule is loose, stitches are used to make it tighter.
Dr. Adam Farber at Phoenix Shoulder and Knee is an expert sports medicine doctor in Tempe, Scottsdale and Phoenix. He offers highly skilled treatment for those suffering from acute or chronic shoulder instability. Call to schedule today!
Resources
Wilk KE, Macrina LC, & Reinold MM (2006). Non-Operative Rehabilitation for Traumatic and Atraumatic Glenohumeral Instability. N Am J Sports Phys Ther, 1(1), 16-31.